I was first diagnosed with breast cancer at the age of 29, just two months after completing an Ironman triathlon and three months before my wedding. At the time, I was focused on my life ahead, and cancer was not a part of the equation.
Fast forward to last year, when I was preparing to celebrate 20 years of breast cancer survivorship, my 50th birthday, and my 20th wedding anniversary. It should have been a time of reflection and joy. My sister had just been diagnosed with breast cancer eight months prior, bringing our family’s genetic link to the disease back into sharp focus. When I found a small lump under the skin of one of my post-mastectomy breasts, I didn’t feel overly concerned—after all, I had undergone prophylactic surgeries, and it had been 20 years since my initial diagnosis. But the biopsy confirmed it: I was facing breast cancer again.
If you’re interested in more personal stories, I’ve written extensively about my journey with breast cancer at various stages, including reflections on 15 years of survivorship
Personal Progress, But Systemic Gaps Remain
Looking back at my first diagnosis at 29, I can see how much has changed in terms of breast cancer treatment. But as I faced my second diagnosis 20 years later, I was reminded of how many of the issues I encountered two decades ago remain. Despite all the pink ribbons and awareness campaigns, too many challenges remain for patients today.
When I underwent chemotherapy for my first diagnosis, I lost all my hair. My husband and I decided to make our wedding, which took place at the halfway mark of chemotherapy, a “wigs optional” event so I wouldn’t feel out of place. By the time of my second diagnosis, cold-capping technology (DigniCap system) had become available, allowing me to keep much of my hair. While I was grateful for this advancement, the emotional toll of visible hair loss was still hard to bear, even if outsiders couldn’t tell I was in treatment.
In addition, research into minimum effective doses for chemotherapy has advanced, reducing short- and long-term side effects for many patients. For those of us with BRCA mutations, PARP inhibitors offer a promising, more targeted treatment option. For non-genetic breast cancers, new treatments like CDK4/6 inhibitors and immunotherapies are providing less invasive solutions for many women.
Reconstructive surgery has also progressed since my first diagnosis. While I didn’t have any surgical decisions to make this time around, I was pleased that my sister had more options for reconstruction than I did. DIEP flap reconstruction–which offers a superior aesthetic outcome and fewer long-term complications–has become more prevalent in the past 20 years. However, this procedure comes with much longer surgeries and recovery times. However, these procedures aren’t accessible to everyone.
Despite these advancements, one reality remains unchanged: mastectomy is still a standard treatment. This underscores the need for continued progress in how we approach breast cancer care.
The Problem with Pink
As Breast Cancer Awareness Month rolls around each year, I can’t help but feel conflicted. While awareness campaigns flood our world with pink each October, they often fail to address the persisting gaps in understanding and care. Yes, awareness has improved—more people are talking about breast cancer, and advances in treatments are saving lives. But for me, the endless pink ribbons and merchandise feel like a distraction from the real conversations we need to be having.
True awareness should go beyond pink merchandise and catchy slogans. It should focus on the misdiagnoses and dismissals that younger women, like me, face when their symptoms don’t fit the typical profile. It should dive into the long-term impacts of breast cancer treatment on a woman’s sexual health, body image, and emotional well-being—areas that are frequently brushed aside. And it must address the disparities in breast cancer care: limited access to early detection tools, lower awareness of breast cancer risks, medical distrust in underserved communities, and barriers to obtaining comprehensive care due to geographic and financial constraints. These gaps mirror broader issues in women’s health care, where concerns are frequently dismissed or minimized, leading to delays in diagnosis and treatment, particularly for women of color and those from lower-income backgrounds. The inequities in breast cancer care reflect broader patterns of neglect and bias in the healthcare system’s approach to women’s health, where gendered assumptions and social determinants of health continue to impact outcomes.
Understanding Hereditary Breast Cancer Risk
There has been a growing emphasis on genetic testing for hereditary breast cancer, particularly for those with a legitimate concern, like my family. With a BRCA1 gene mutation, I’ve been fully aware of my heightened risk, as was my sister. However, it’s a common misunderstanding that a family member’s breast cancer diagnosis automatically increases your personal risk. In reality, only about 5-10% of breast cancers are caused by inherited genetic mutations such as BRCA1 or BRCA2.
While genetic testing is critical for those at higher risk—especially for groups like Ashkenazi Jews, who are more likely to carry these mutations—most people with a family history of breast cancer won’t necessarily develop the disease. This distinction is important and should be better communicated in awareness campaigns.
Even without a BRCA mutation, having a family history does entitle individuals to regular and advanced screenings, such as ultrasounds and mammograms. Just because you don’t have the BRCA gene doesn’t mean there isn’t another genetic or shared environmental risk at play, even if the specific determination is unknown. Screening saves lives, and women should be encouraged to undergo as much of it as possible. Understanding your own breast cancer risk and staying proactive with screenings are key steps in prevention and early detection.
Breast Cancer Risk by Age and Other Significant Factors
Breast cancer risk naturally increases with age. For example, the chance of being diagnosed with breast cancer over the next 10 years is about 0.49% for women in their 30s but rises to 4.09% for women in their 70s.
While age is an important risk factor, cancer is a multifactorial disease, meaning it arises due to a combination of factors, many of which are beyond an individual’s control. These factors include genetics, hormones, and environmental influences. While lifestyle choices can influence risk, they do not guarantee prevention. In fact, many people who lead healthy lifestyles still develop breast cancer. Avoiding a blame-based narrative around the disease is critical, as no one can fully control their risk.
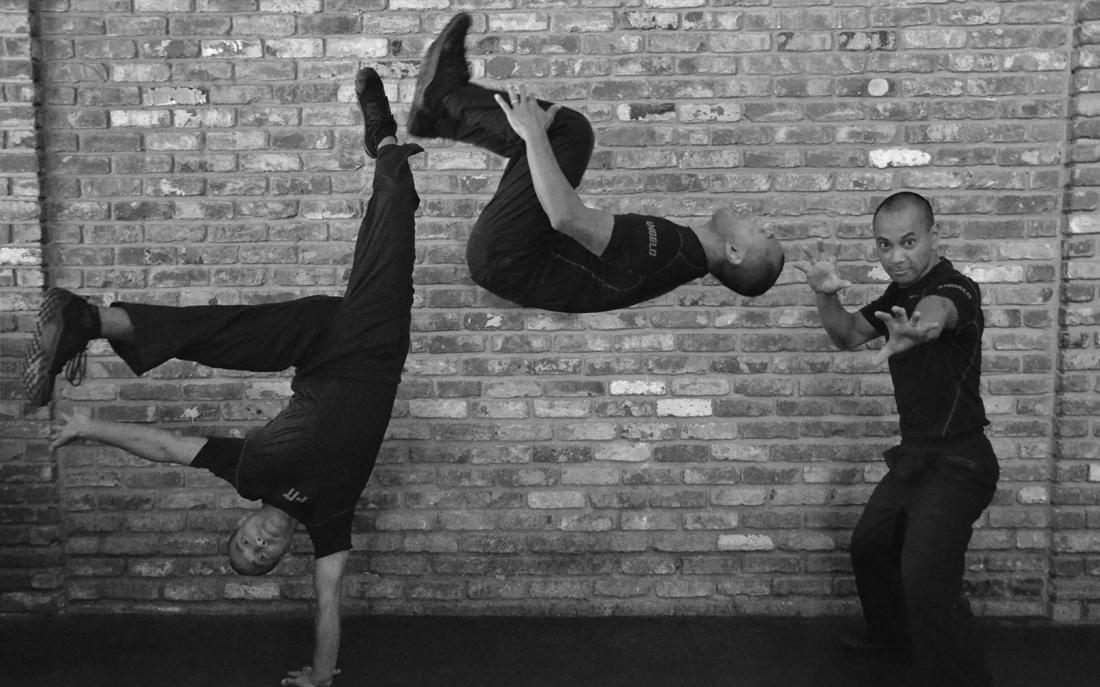
However, we do have some control over modifiable risk factors. Regular physical activity, maintaining a healthy weight, and limiting alcohol intake can help reduce the likelihood of developing breast cancer. For instance, postmenopausal women who are physically active and maintain a healthy weight can reduce their risk by 20-40%, while consuming alcohol regularly increases risk by about 10% for each daily drink. While no lifestyle choice can guarantee prevention, they definitely contribute to overall well-being and breast cancer prevention.
A Call for Real Change
Reflecting on my two diagnoses, I see both progress and stagnation. I’m grateful for the advancements that have allowed me to continue living a full life, but I can’t help but feel we need to shift the conversation.
Celebrating survival is not enough; we must focus on quality of life after treatment. Real awareness involves addressing the short- and long-term emotional, physical, and sexual side effects of breast cancer diagnosis and treatment while ensuring that every woman receives compassionate, comprehensive care that prioritizes her overall well-being during and after treatment. It also means calling for equitable access to life-saving treatments, especially for underserved communities.
As I approach the 20th anniversary of my first diagnosis, I’m reminded of how far we’ve come—and how far we still need to go. The pink ribbons I see everywhere should be more than a symbol—they should remind us of the real, ongoing need for meaningful, systemic change.
FAQs
What are the signs of breast cancer in younger women?
While breast cancer is more common in older women, younger women may experience symptoms such as lumps, nipple discharge, or changes in breast shape or size. Regular self-exams are crucial.
Does having a family history of breast cancer increase your risk?
Yes, a family history can increase risk, but most breast cancers are not inherited. Genetic mutations, like BRCA1 or BRCA2, account for only 5-10% of cases.
How has breast cancer treatment improved over the years?
Treatments have become more targeted with advancements like PARP inhibitors for BRCA mutations and CDK4/6 inhibitors for non-genetic cancers, reducing side effects and improving outcomes.
What is the importance of screening for breast cancer?
Screening is essential for early detection, which can significantly improve outcomes. Regular mammograms, ultrasounds, and genetic testing (when appropriate) are critical tools.
How can lifestyle changes reduce breast cancer risk?
Maintaining a healthy weight, exercising regularly, and limiting alcohol consumption can help reduce risk. However, lifestyle changes alone cannot eliminate risk entirely.
Is mastectomy still a standard treatment for breast cancer?
Yes, mastectomy remains a common treatment, especially for those at high genetic risk. However, reconstructive options have improved significantly in recent years.