Menopause is the second most drastic hormonal transition women will experience throughout their lifetime, and yet the experience can be vastly different between individuals. Some have extreme side effects and symptoms while others hardly remember it’s happening and yet they are all going through the same hormonal dip and withdrawal. This change marks the end of reproductive age and ability as well as a significant pivot in many other health aspects, including energy, metabolism, bone density and structure, digestion, immunity, and sleep health.
Menopause Defined
Some of the most common symptoms experienced during menopause include hot flashes, night sweats, mood swings, irregular periods and weight gain. Some lesser known symptoms include reduced sex drive/low libido, heightened anxiety and depressive symptoms, brain fog and mental fatigue, and identity crisis (Mehrnoush et al, 2021; De Franciscis et al, 2019). For many women, this is an incredibly frustrating and confusing time, as they are experiencing so much change physically and emotionally during this transition period to menopause and postmenopause.
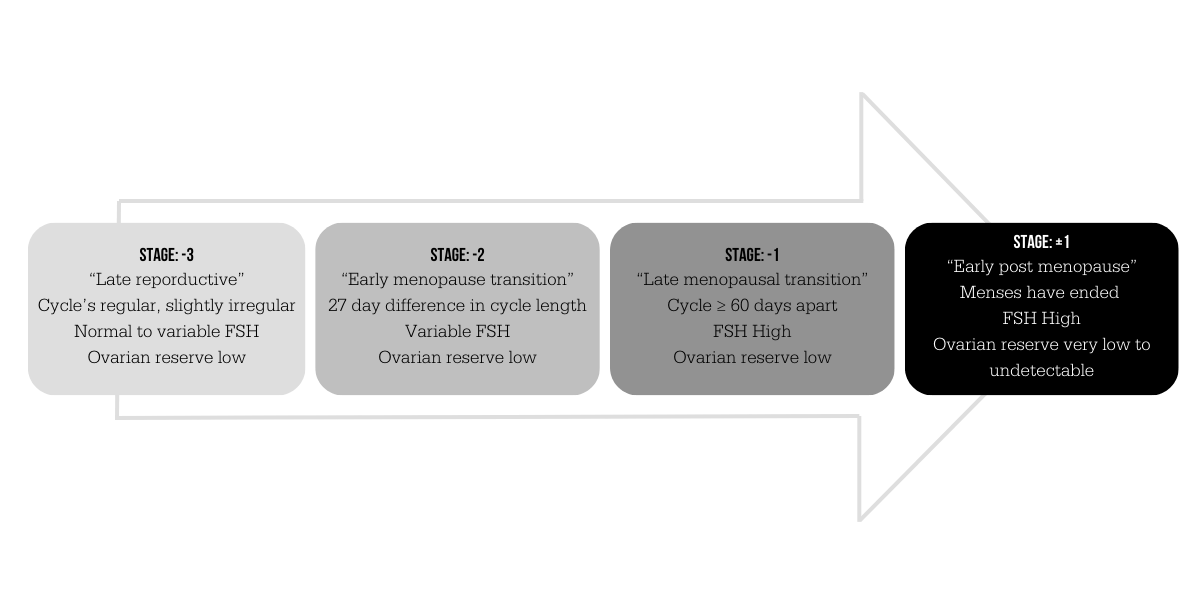
Many women experience a wide range of symptom severity through the pre- and peri-menopausal phases. As women age, specific reproductive hormones decrease, which causes a reduction in processes like egg maturation and hormone production and follicle stimulation. But each month, the level of hormone present will determine the severity of symptoms, and the total maturation status of the follicle is the primary component of this change. Because there are many hormones involved in this change, they are competing with one another, and can often cause symptoms to become wild and unpredictable for quite some time. There are technically four phases of menopause, as outlined below… (Santoro et al, 2021
- Late reproductive stage
- Defined by mostly regular cycles, with some slight irregularity appearing occasionally
- Follicle stimulating hormone (FSH) is normal or starts to slightly vary from normal
- Low egg count
- Early menopausal transition
- >/= 7 day difference in cycle lengths
- First obvious sign: skipped cycle
- Shorter cycles more common
- Variable and irregular FSH levels
- Lower total egg count
- Late menopausal transition (generally lasts 1-3 years)
- Cycles are >/= 60 days apart
- Variable and highly irregular FSH levels
- Lowest egg count
- Early post-menopause
- Cycles have ended (timing determined 1 year after last cycle)
- FSH levels are high
- No detectable egg or follicle count
Because of the wild and unpredictable nature of the hormone levels throughout these transitions, many doctors and functional medicine providers recommend hormone replacement therapy (HRT) (Mehrnoush et al, 2021). Hormone replacement therapy is using bio-identical and/or synthetic hormones to regulate the levels of hormones and ease the transition through each phase. The hormones in our bodies have positive and negative feedback loops intertwined into them, and when these hormones are not at consistent levels, it can cause downstream effects in other hormone pathways and processes throughout the body, such as the vasomotor symptoms in menopause. HRT acts on these feedback loops to reduce and diminish the disruption to these levels and stabilize symptoms experienced by the patient. Oftentimes, providers monitor hormone levels throughout treatment and will adjust if negative side effects are experienced.
Additionally, this hormonal regulation can be beneficial for many systems at once – metabolism stabilizes, mood stabilizes, sleep becomes more regular, bone density is preserved, and muscle is maintained (Juppi et al, 2020). When combined with exercise, women can push off years of bone density loss and create a positive change in their aging. Like any treatment, there are some precautions to be aware of, and you should consult a physician for medical and health advice. Those with any family or personal history of breast cancer, ovarian cancer, endometriosis, bone cancers, thyroid issues, endocrine disorders, heart issues or heart disease, or any other chronic hormonal disruption should be cautious when approaching HRT, and may not qualify for HRT because of these conditions (Santoro et al, 2021).
Some factors that affect menopausal symptom severity…
- Obesity status and BMI
- Race/ethnicity
- Smoking
- Previous hormonal diagnoses
There are many ways to combat the symptoms and side effects of menopause. Due to the complexity of this experience, it’s hard to know what will work for everyone. Use your symptoms as a guide, and be diligent about tracking any changes (and collecting data over time for your very own n=1 experiment!). One of my favorite apps Clue has a menopausal mode to track any symptoms or changes in symptoms over time. Plus, this app is one of the only available on the market that actually protects your health data! Here are some helpful and unique ideas for addressing menopause symptoms…
Activity
Both cardiovascular and resistance training show beneficial effects on preserving muscle mass and conditioning through the menopausal transition. The maintenance of the muscle tissue allows for preservation of metabolism and aids in maintaining hormonal status as well (Juppi et al, 2020). Though there is a muscle type shift through menopause, where we see a shift of some Type 2 muscle (fast-twitch muscle) to type 1 muscle (slow-twitch muscle) regardless of HRT status, it’s important to continue training both energy systems.
Resistance training starting in adulthood and continued through the menopausal transitions helps to reduce vasomotor symptoms and normalize luteinizing hormone levels (Nilsson et al, 2022). Additionally, the resistance training can help with preserving bone density and limit fracture risk through menopause and postmenopause, one of the most common and significant downstream effects of the menopausal transition.
Eating Strategy
Prioritizing healthy fats, lean protein, complex carbs, and high vegetable content can help with reducing menopausal symptom severity through these transitions. Omega-3 fatty acids help with hormone production, inflammation regulation, skin and hair health, and cognitive function. Flax seed is a great way to help support skin, hair, and nails against becoming brittle and dry. One eating strategy that is particularly researched for its efficacy in managing menopausal symptoms – the Mediterranean diet. Because of its reliance on healthy fats, high fiber from fruits and veggies, lean proteins, and complex carbs, it provides all the nutrients for your body to mitigate excess undue stress from the menopause transition. In addition to the nutrient density of the Med Diet, there are other benefits from the mediterranean diet, including cholesterol management, blood pressure management, and weight management (Silva et al, 2021).
Hydration and Electrolytes
Hydration is incredibly important for flushing out toxins and metabolites, but also maintaining good hydration of tissues, maintaining circulation and body temperature, and promoting electrolyte/fluid balance. It is also vital to maintain a healthy balance of electrolytes, not only for the fluid/electrolyte balance, but for adrenal function. A broad spectrum electrolyte works well for metabolic support, hydration and fluid balance, immune function, and bone maintenance. Here are a few of my favorites!
- Ultima Broad Spectrum Electrolyte Powder – 0g sugar, great flavors!
- ConcenTrace Mineral Packets – includes B vitamins, zinc, and vitamin C for immune support
Supplements and Herbal Medicine
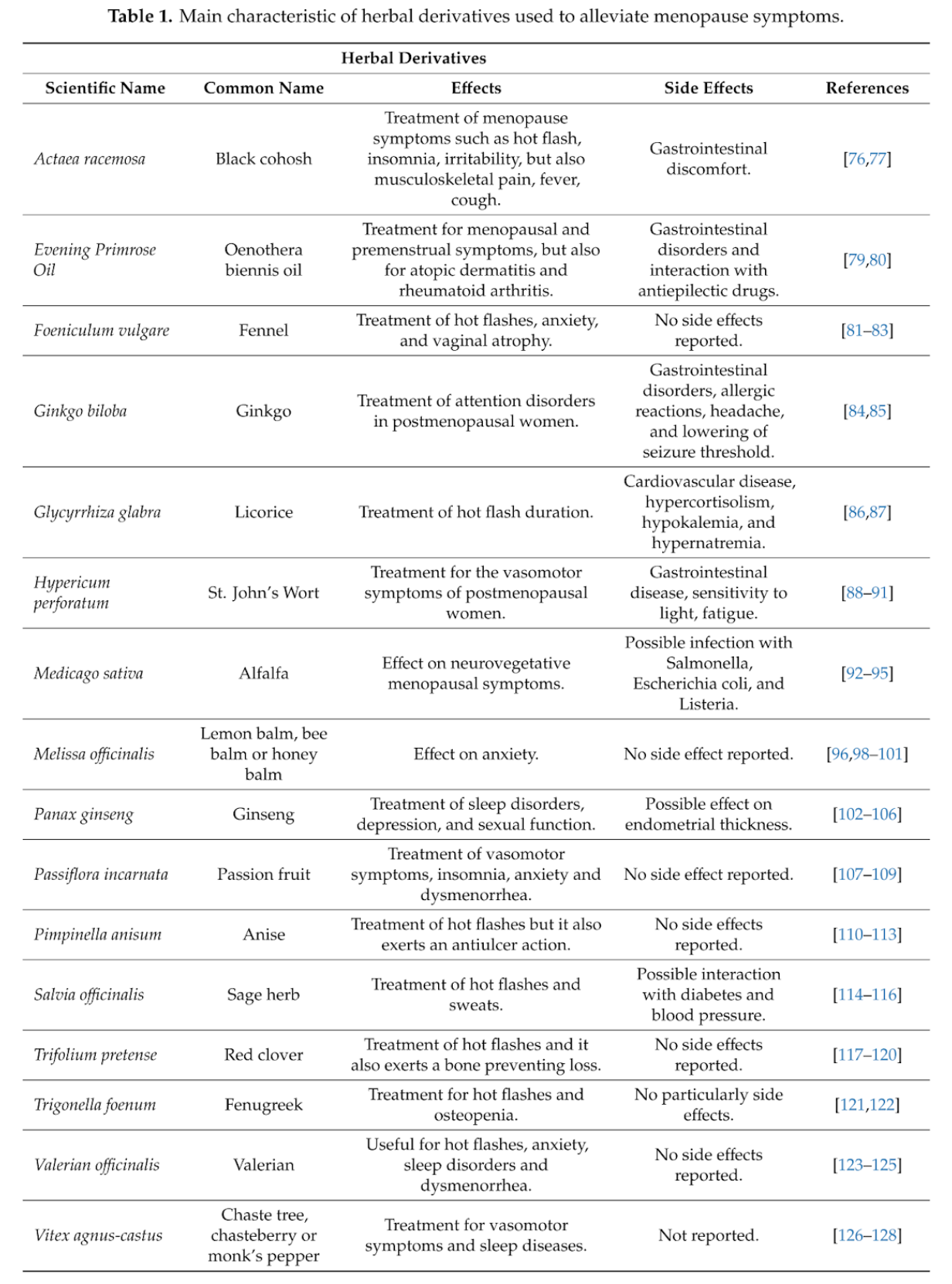
Ginkgo, lemon balm, and St. John’s wort have all proven to be effective against menopausal symptoms, including brain fog, migraines/headaches, low energy, and depression (De Franciscis et al, 2019). Flax seeds contain phytoestrogens that help with moderating menopausal symptoms, particularly night sweats, hot flashes, and dryness. Maca, when used appropriately, can be a great herb for night sweats, energy level, hormone status, and especially libido and sexual function in women. One caution with maca, if there is any history of breast cancer, reproductive cancers, or PCOS, please speak with your physician before using.
Regular whole-system treatment can help to create balance throughout the body and regulate the body’s response to the transition changes over time. Practices such as acupuncture, traditional chinese medicine, reflexology, yoga, and mindfulness can make a lasting impact on health metrics and symptoms as well!
Stress Management, Counseling, and Support Groups
In a few studies, cognitive behavioral therapy has proven to be an effective strategy for combating not only the mental health component, but certain physical symptoms as well. Because many of the vasomotor symptoms happen more when we’re stressed, certain stress management strategies can actually reduce physical symptoms like night sweats, hot flashes, and mood swings.
Through this transition, women often experience reduced libido or sex drive, caused by the hormone fluctuations, lack of sleep and energy, and not fully understanding everything happening within their bodies. Mindfulness exercises and yoga have been shown to increase sexual desire and overall sexual health in perimenopausal and postmenopausal women, more so than physical activity or eating strategy adjustments (Carcelén-Fraile et al, 2020).
del Carmen Carcelén-Fraile, M., Aibar-Almazán, A., Martínez-Amat, A., Cruz-Díaz, D., Díaz-Mohedo, E., Redecillas-Peiró, M. T., & Hita-Contreras, F. (2020). Effects of physical exercise on sexual function and quality of sexual life related to menopausal symptoms in peri- and postmenopausal women: A systematic review. In International Journal of Environmental Research and Public Health (Vol. 17, Issue 8). MDPI. https://doi.org/10.3390/ijerph17082680
De Franciscis et al, A nutraceutical approach to menopausal complaints (2019).
Juppi, H. K., Sipilä, S., Cronin, N. J., Karvinen, S., Karppinen, J. E., Tammelin, T. H., Aukee, P., Kovanen, V., Kujala, U. M., & Laakkonen, E. K. (2020). Role of menopausal transition and physical activity in loss of lean and muscle mass: A follow-up study in middle-aged finnish women. Journal of Clinical Medicine, 9(5). https://doi.org/10.3390/jcm9051588
Kemmler, W., Shojaa, M., Kohl, M., & von Stengel, S. (2020). Effects of Different Types of Exercise on Bone Mineral Density in Postmenopausal Women: A Systematic Review and Meta-analysis. In Calcified Tissue International (Vol. 107, Issue 5, pp. 409–439). Springer. https://doi.org/10.1007/s00223-020-00744-w
Mehrnoush, V., Darsareh, F., Roozbeh, N., & Ziraeie, A. (2021). Efficacy of the Complementary and Alternative Therapies for the Management of Psychological Symptoms of Menopause: A Systematic Review of Randomized Controlled Trials. Journal of Menopausal Medicine, 27(3), 115. https://doi.org/10.6118/jmm.21022
Nilsson, S., Henriksson, M., Berin, E., Engblom, D., Holm, A. C. S., & Hammar, M. (2022). Resistance training reduced luteinising hormone levels in postmenopausal women in a substudy of a randomised controlled clinical trial: A clue to how resistance training reduced vasomotor symptoms. PLoS ONE, 17(5 May). https://doi.org/10.1371/journal.pone.0267613
Santoro, N., Roeca, C., Peters, B. A., & Neal-Perry, G. (2021). The Menopause Transition: Signs, Symptoms, and Management Options. In Journal of Clinical Endocrinology and Metabolism (Vol. 106, Issue 1, pp. 1–15). Endocrine Society. https://doi.org/10.1210/clinem/dgaa764
Silva, T., Oppermann, K., Reis, F., & Spritzer, P. (2021). Nutrition in Menopausal Women: A Narrative Review. Nutrients, 13. https://doi.org/10.3390/nu13072149.
Sign up for FiT’s Health Optimization and Wellness Blog
![]() 600 Rancho Shopping Center, Los Altos CA 94024. | 650-947-9831
600 Rancho Shopping Center, Los Altos CA 94024. | 650-947-9831
Get Directions | Email Us | Jobs | Follow us: