Menopause Doesn’t Have to be Miserable
Menopause is something that all women experience but is seldom a topic of discussion over coffee with friends. And little is offered by the medical profession to help us manage or even flourish during this period of our lives, which can last from our mid-forties to our sixties. For the most part, we are told to grin and bear it with many doctors being reluctant to prescribe hormones except for the most severe symptoms of hot flashes; however, when properly prescribed and monitored, bioidentical hormone replacement therapy (BHRT) can mitigate hot flashes, alleviate night sweats, clear brain fog and prevent weight gain. Hormones can improve libido and increase sexual fulfillment. If you are thinking, ‘sounds too good to be true’ or ‘what’s the catch?’ keep reading as this life changing therapy, once thought to increase risk of a variety of diseases, is actually quite safe and believed to reduce disease risk for the large majority of women.
Busting Myths about Hormone Replacement Therapy (HRT)
I’ve been prescribing bioidentical hormones for several years now and am amazed that there is still so much controversy and misinformation surrounding this topic. The following beliefs are commonly-held but should be relegated to the realm of myth.
Myth #1: Hormone Replacement therapy is dangerous and causes cancer
The Women’s Health Initiative (WHI) study from 1991 did women a huge disservice. The study was terminated early when women on hormone replacement were found to have higher rates of breast cancer and heart disease than women not on hormones. As a result of this study, doctors stopped prescribing hormone replacement therapy to women. Currently nationwide, less than 10% of eligible women take hormones in menopause. Hundreds of women are missing out on a potentially life-changing treatment. This trend is starting to change as other studies emerge and more practitioners are taking a critical look at the fine points of the data.
Here’s what menopausal women need to know: the hormones that were used by women in the study were synthetic hormones given orally (more on this significance soon). Further, when you compare study groups, the women taking synthetic progesterone developed more breast cancer and heart disease. The women in the estrogen-only arm actually had lower rates of breast cancer notwithstanding that the estrogen was synthetic. Here’s the press release: “The NIH has concluded that with an average of nearly 7 years of follow-up completed, estrogen alone does not appear to affect (either increase or decrease) heart disease, a key question of the study. It has not increased the risk of breast cancer during the time period of the study.”
Based on other studies like the French E3N cohort study, which looked at 80,000 French women over a period of 12 years, hormone replacement therapy, if given properly in the correct form and with careful monitoring, does not increase breast cancer risk. Many other studies have proven the safety of BHRT showing no increased risk for heart disease, strokes and blood clots.
Myth #2: Bioidentical and synthetic hormones are equivalent
Bioidentical hormones are structurally identical to the endogenous hormones produced by your body. They are derived from plant-based sources like yams. Synthetic hormones on the other hand, have additional chemical molecules, or parts of molecules to be exact, attached to their structures– they are foreign substances to the body. Estrogen is made from pregnant mare’s urine; synthetic progesterone, or progestin is made in the lab and was originally designed to be used primarily for birth control purposes, not to relieve menopausal symptoms.
Prometrium, or micronized progesterone, is the bioidentical form of progesterone that is the safest to take. In fact, it is most certainly associated with a lower risk of breast cancer and heart disease than synthetic progestin. Based on the findings from the WHI study above, methoxyprogesterone (synthetic progestin) should not be taken for hormone replacement.
Estrogen comes in three forms: Estrone or E1, Estradiol or E2 (the most abundant form in the body) and Estriol or E3. Bioidentical estrogen is given as either estradiol (E2), estriol (E3) or a combination of the two called Biest. Estrone is quite potent and has a high affinity for breast tissue cellular receptors. As we can derive all the desired clinical benefits from the combination of estradiol and estriol, estrone should be avoided in HRT.
In summary, bioidentical hormone replacement therapy (BHRT) is safer than synthetic and the safest hormones to take are estradiol, a combination of estradiol and estriol (Biest), and prometrium (micronized progesterone).
Myth #3: All delivery forms of hormone replacement are alike
When taken orally, estrogen gets metabolized by the liver and can generate pro-cancerous metabolites, therefore estrogen should be delivered through the skin to avoid this. Bioidentical estrogen is available in a patch, a cream, a vaginal suppository or in pellet form*. Of these options, the only bioidentical estrogen that’s mass produced by the pharmaceutical industry is the patch (called Vivelle, or Climara); the cream or suppositories can be prepared by a well-reputed compounding pharmacy; pellets are administered by the practitioner, however, pellets are long acting (3 months) so can make initial titration difficult while trying to achieve maximum efficacy with minimum dose. My preference is to start with a patch, cream or vaginal option at least until optimal dosage is determined at which point making the switch to pellets is fine and can aid with compliance for those who find the daily routine of administering HRT challenging.
Progesterone can be taken orally or topically as long as it is bioidentical prometrium as opposed to progestin. Progesterone metabolizes into a nice calming metabolite, so it can help with sleep and anxiety if taken right before bedtime. It is made by a pharmaceutical company in a 100 mg dosage form; compounding pharmacies are used if higher or lower dosages are desired.
Testosterone, like estrogen, should be given topically. It comes in a cream, vaginal suppository or pellet. Conventionally trained physicians don’t prescribe testosterone. Because of my own lack of knowledge of the benefits of testosterone for the human body and images I had of bodybuilders bulking up with testosterone, I used to be cautious about using it as well, but it is an important hormone for maintaining bone density and enhancing cognition and memory. It’s also key for a healthy libido and preserving lush hair and moist skin.
*Note of caution regarding buccal troches—these are small tablets that you place in your cheek that supposedly dissolve into your skin. Because it is dissolving in your mouth, there is a risk that you swallow some hormone, and thus end up getting oral estrogen, which, as stated above, should be avoided.
Myth #4: Women should stay on hormone replacement only for symptom relief and for the shortest time possible
With what we now know to be truth vs. myth, the benefits of BHRT far outweigh the risks for the large majority of women. Because conventional physicians prescribe synthetic hormones with a higher risk of breast cancer, clots and heart disease, the teaching was always to use the lowest dose of hormones for the shortest amount of time (ideally less than five years). However, there is more and more data on the benefits of hormones for women, especially in preserving cognition and lowering the risk of Alzheimer’s disease. Improvements to skin, hair, quality of life, sleep, libido, bone health and cognition, are also noted as benefits to long-term use of BHRT. Good news is that there is no need to stop once you start as long as you are feeling well and are being monitored carefully!
Myth #5: You don’t need to measure hormone levels while replacing hormones. Blood tests can be used and should be sufficient.
Practitioners have widely differing ways of prescribing hormones. Some prescribe and dose by symptoms rather than by checking hormone levels, i.e., if your hot flashes disappear then you are on the correct dose. This might be fine, but women in general feel so good on hormones they can be unintentionally over-replaced. Often too, below-normal levels and above-normal levels of the same hormone can cause identical symptoms, so unless you measure, you won’t know the exact cause of the symptoms. Finally, the overall goal of BHRT is not to create a virile Lara Croft, but a nice and healthy 40+ year-old gal.
Checking hormone levels is important to achieving the proper balance. Accepted, tried and true hormone testing should be done with saliva, capillary blood or urine. Blood tests will not reflect tissue levels of topically-applied hormones. Well reputed companies for testing are ZRT, Genova and Dutch Labs.
My approach is to get baseline levels before starting BHRT to help determine starting doses. Since it takes about three months for hormone receptors to saturate, I check follow-up hormone levels 3 months later, at which point dosages may need to be tweaked. Once the desired hormone balance is achieved, I continue to check annually to ensure stability. This is a long and time-consuming process and can be somewhat costly to the patient, but it is safer in the long-run.
Myth #6: Any alternative medicine practitioner can prescribe HRT well
Every woman is different and will have a different hormonal balance and symphony that needs to be carefully titrated. Like any prescription, improper dosing can lead to doing more harm than good. A knowledgeable, well trained practitioner who closely monitors levels and adjusts dosing accordingly is imperative for BHRT to be both safe and effective. Look for a practitioner who has completed fellowships in alternative medicine or integrative medicine, has completed the American Academy for Anti-Aging Medicine’s (A4M) mini-fellowship in hormone replacement and/or has additional formal training in hormone replacement therapy.
Before I trained in bioidentical hormones, I felt I didn’t have the adequate knowledge-base to proceed with safely prescribing hormones; it was a big black box and hormones seemed scary to me because of their reputation from the WHI study. I think this is a fear shared by most conventionally-trained physicians who would start prescribing if they pursued proper training in this field, which takes interest, time, energy and resources that already busy primary care doctors don’t often have. When doctors see that their patients are benefitting from BHRT, my hope is that more conventionally-trained ob gyns, internists and family practitioners will pursue appropriate training to prescribe it.
Myth #7 BHRT is the only thing needed to make you feel better
BHRT can go a long way to improving quality of life. But it is important to remember that pills and patches alone are still not enough. Other important hormones to look at are cortisol and thyroid, so a thorough practitioner will be measuring these as well. If cortisol is too high from stress, hormone balancing will not be optimal. Replacing hormones in someone with high stress levels will only lead to more cortisol production and not the desired hormone augmentation (something called cortisol steal) and will backfire.
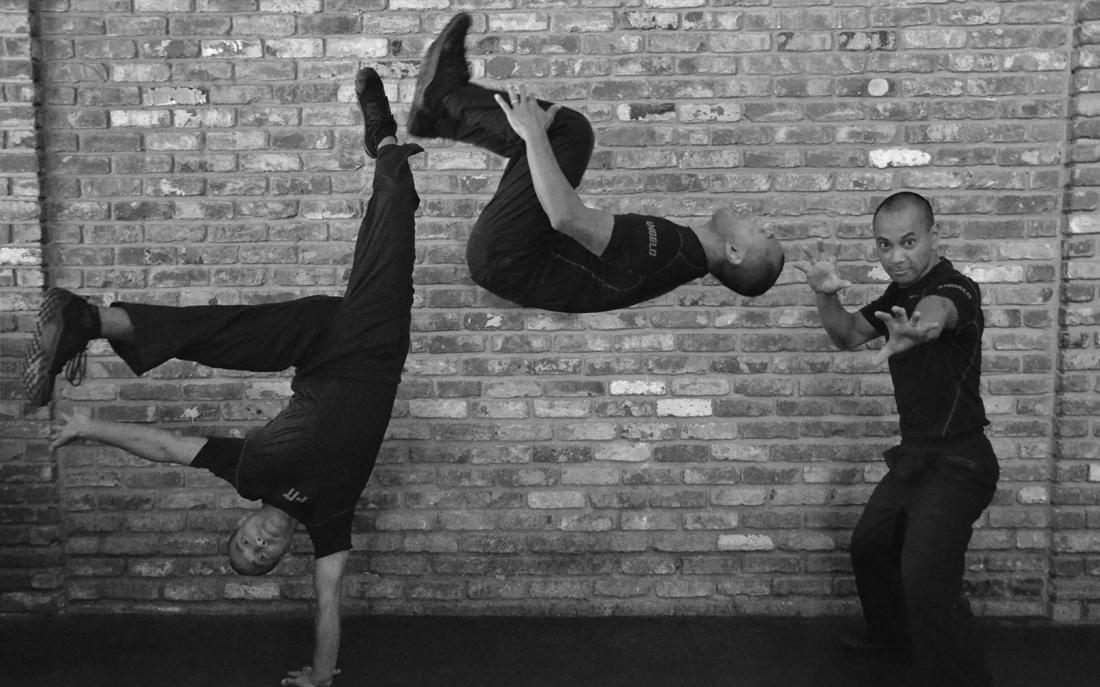
Stress management with meditation, yoga, deep breathing and exercise are key, as are good sleep, a healthy diet and a balanced lifestyle. Working in concert with your physician and partnering with knowledgeable fitness professionals like those at FiT in Los Altos, where they take a holistic, comprehensive approach to optimizing health is ideal. No amount of hormones will help you feel better if you are chronically sleep deprived, consistently drink 2 glasses of wine a night and stay glued to your sofa. BHRT should be a compliment to an already healthy and active lifestyle to help keep you that way as long as possible.
7 Things You Now Know about BHRT:
The saying goes something like, ‘Growing old isn’t for the weak but it sure beats the alternative.’ Appropriate hormone therapy can take some of the wind out of aging’s sails and improve quality of life. Here are the most important thing for you to remember:
- Most menopausal women are good candidates for hormone replacement therapy
- Hormone replacement therapy can mitigate symptoms such as: poor sleep quality, hot flashes, low or absent libido, brain fog, hair thinning/ hair loss, dry eyes and dry skin, mood swings, and anxiety
- BHRT is safer than synthetic hormone replacement in terms of breast cancer and heart disease risk and can lower the risk for cognitive impairment
- Optimal delivery form varies by hormone type- estriol, estradiol and testosterone should be administered topically or by suppository; bioidentical prometrium can be taken orally or topically in a cream. Once optimal dosing is achieved, pellets are a viable delivery form.
- Initial dosing should be closely monitored until balance is restored then checked annually
- BHRT can be used indefinitely. There is no upper age limit
- Lifestyle factors (eating strategy, sleep hygiene, stress management, exercise prescription and self care) affect hormone balance and should be addressed along with BHRT
In summary, BHRT may open up a new world of benefit for women and I encourage you find out more and educate yourself. Some questions you might want to ask your health care practitioner include:
- Based on my age and family history, when can I expect symptoms of perimenopause or menopause?
- What can I do to relieve and address my menopausal symptoms such as hot flashes, insomnia, low energy, vaginal dryness or decreased sexual desire?
- How do you test hormone levels? What tests do you use and why?
- What is your philosophy about hormone therapy? What can you tell me about natural or bioidentical hormones?
- Am I a candidate for bioidentical hormones?
- If I choose hormone therapy, are there different ways I can take them such as capsules, topical creams, vaginal creams or suppositories? What are the advantages or disadvantages to these different options?
- What are my risk factors for breast cancer, heart disease and osteoporosis, and what can I do to prevent these problems?
- How often should I get a mammogram, clinical breast exam and pap smear?
- Are there foods, nutritional supplements, and herbs that can help with symptoms and address health problems?
- What types of exercise and lifestyle changes will keep me healthy?
To learn more about BHRT, here are two helpful books:
- The Hormone Cure: Reclaim Balance, Sleep and Sex Drive; Lose Weight; Feel Focused, Vital, and Energized Naturally with the Gottfried Protocol Paperback – March 11, 2014,by Dr. Sara Gottfried
- What You Must Know About Women’s Hormones: Your Guide to Natural Hormone Treatments for PMS, Menopause, Osteoporosis, PCOS, and More, by Dr. Pamela Smith
About the author: Dr. Yumi Ando is a Stanford-trained Internal Medicine physician, and is also Board-certified in Integrative Medicine. She tries to combine the best practices of conventional Western Medicine with those of Eastern and Integrative Medicine to care for patients holistically and to optimize quality of life.